Hemobartonellosis in cats is a life-threatening infectious disease. Its appearance is provoked by a specific type of rickettsia, which veterinarians call Bartonella. They lead to severe dysfunction of the animal's metabolic system and a lack of oxygen in the blood. At the same time, the cat rapidly loses weight, and its internal organs change pathologically.
The insidiousness of the infection is manifested in the fact that a cat can be infected with hemobartonellosis for a long time, acting as a carrier of the disease, but the disease will not manifest itself in any way on the carrier. According to statistical data, only 30% of representatives of the cat family have pathology with pronounced clinical symptoms. The article will discuss the causes and symptoms of the disease, methods of its treatment, as well as whether feline hemobartonellosis is dangerous for people.
What is hemobartonellosis
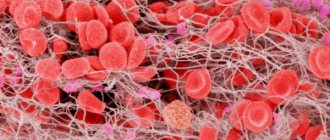
The causative agent of infectious anemia is feline hemobartonella, or Haemobartonella felis. This is a hemotrophic bacterium in the form of a grain that does not have a shell. It parasitizes on the surface of the red blood cell, attaching to the outer membrane. Damaged cells are destroyed by the spleen and removed from the bloodstream. An infected cat develops anemia, or anemia. Due to a lack of red blood cells, the oxygen supply to all internal organs is disrupted, which leads to a weakening of their functions. Prolonged hypoxia causes tissue death, which threatens the life of a pet and requires urgent medical attention.
Hemobartonellosis affects red blood cells, which are removed from the bloodstream by the body, causing anemia
The microorganism Haemobartonella felis occupies an intermediate position between mycoplasmas and rickettsiae. This blood parasite does not live outside the cat's body, so it cannot be studied in the laboratory. There is no reliable information about how the pet’s immune system protects after infection with hemobartonellosis. Veterinarians know of cases where the pathogen is present in the animal’s bloodstream and does not cause anemia. But most cats become seriously ill when the parasite cannot be destroyed.
Feline hemobartonella does not affect other animal species or humans.
Differential diagnosis of feline hemobartenellosis
Other blood-parasitic diseases of cats can occur with similar clinical symptoms, such as Babesia spp. (widespread in Africa, not found in our latitudes) Cytauxzoonoses felis found in the USA, the natural reservoir is the red lynx. This must be kept in mind when treating animals brought from abroad.
In addition, diseases associated with oxidative damage to red blood cells occur with similar symptoms, for example, poisoning of cats with onions or acetaminophen (paracetamol). These toxic substances, when ingested by a cat, lead to the accumulation of methemoglobin in red blood cells (oxidized hemoglobin incapable of carrying oxygen), the formation of Heinz bodies (inclusions in red blood cells consisting of oxidized hemoglobin), hemolysis and a sharp decrease in the oxygen capacity of the blood, leading to hypoxia.
Many immune-mediated autoimmune diseases can lead to hemolysis; blood parasites themselves can serve as a trigger for the occurrence of autoimmune hemolytic anemia.
In addition, DIC syndrome (disseminated intravascular coagulation, consumption coagulopathy, thrombohemorrhagic syndrome) is also often accompanied by anemia.
Causes of infection
A domestic cat runs the risk of becoming infected with hemobartonellosis only after contact with the blood of a sick animal or carrier of the infection:
- Most often, the pathogen enters the body of a healthy pet through flea and tick bites. They serve as vectors or temporary hosts for Haemobartonella felis.
- Wounds inflicted by animals in a fight also become one of the ways of infection.
- It is possible that a cat may become infected through a donor blood transfusion. This rarely happens, because animals are required to be checked for carrier status.
In the asymptomatic form of the disease, there are no clinical signs of anemia, so the cat appears to be healthy . But during pregnancy the parasite becomes more active. Hemobartonella crosses the placenta and causes the death of kittens . They are born dead.
Most often, young cats under three years of age suffer from infectious anemia, and the disease is acute and severe. In cats, hemobartonellosis usually occurs in a chronic form. In this case, a decrease in the body's resistance due to unfavorable factors aggravates the disease.
The risk of hemobartonellosis in cats is affected by:
- malnutrition;
- tumor process;
- surgical intervention;
- stressful situation;
- addition of another infection.
Symptoms of hemobartonellosis in cats
Symptoms will not appear immediately. The incubation period for feline infectious anemia is 7-14 days. Owners begin to notice that their four-legged pet is losing weight before their eyes, becomes lethargic, apathetic, gets tired quickly and moves little. These symptoms are inherent in many cat diseases, specifically for hemobartonellosis:
- difficulty breathing;
- tachycardia;
- lack of appetite;
- damage to the skin (bite marks, scratches, wounds, inflamed areas of the skin, suppuration);
- darkening of urine;
- slight hyperthermia (a strong increase in temperature is observed in rare cases);
- yellowness with an orange tint of the skin due to oxygen starvation;
- pale gums, often with a lemon tint;
- the skin loses elasticity, becomes dry, stretches and sticks tightly to the muscles;
- the cat's voice becomes hoarse;
- dullness and disheveled fur;
- the appearance of strange taste preferences, for example, a craving for chalk, sand, ash, garbage, dirt.
INTERESTING TO KNOW: Why do cats get flatulence?
In severe cases of blood parasitic disease, dehydration, exhaustion, and dystrophy are observed.
If the disease occurs in a latent form, this does not mean that disturbances do not occur in the pet’s body. Infections are already wreaking havoc, and the consequences may be irreversible.
If your pet has been bitten by ticks or fleas, be careful; it is possible that he may already be developing hemobartonellosis. Don't risk it - take your cat to the veterinarian.
Symptoms of the disease in cats
From the moment of infection to the onset of the first symptoms of hemobartonellosis, 8–17 days pass. The domestic cat becomes weak and sleeps more. When he starts playing, he quickly loses interest and leaves. Doesn't respond to his name. When your pet yawns, it becomes noticeable that his gums and tongue are pale pink, almost white. A healthy animal's tongue is dark pink, making it the most accurate indicator of anemia.
If anemia is suspected, a cat's tongue should be checked first - pallor of the mucous membranes is a clear symptom of hemobartonellosis
During physical activity, the animal quickly gets tired and breathes with its mouth slightly open. Tachycardia appears with a pulse rate of more than 180 beats per minute. With prolonged hypoxia, it is noticeable even in a calm state. From the appearance of a large amount of hemoglobin in the liver, inflammation begins, the skin and mucous membranes turn yellow. The color of the urine darkens and a brown tint is added (microglobinuria). The animal's appetite decreases and food selectivity appears. The pet's coat becomes disheveled and thins in some places due to dry skin.
Regenerative anemia and lack of body weight are the most characteristic signs of hemobartonellosis. However, in adult cats the disease sometimes manifests itself as inflammation of the testicles. Body temperature usually does not rise, but in acute cases fever occurs. It indicates severe intoxication of the pet’s body, requiring immediate medical attention.
Signs and symptoms
Diseases from cat scratches
It is an infectious disease with symptoms that can range from mild to severe. Although in most patients the disease resolves spontaneously within 2-4 months without treatment, in other cases, antibiotic treatment is recommended for people with suppressed immune systems such as HIV/AIDS.
The main symptoms of cat scratch disease may not appear for several days or weeks after infection. A red spot may appear on the skin at the site of infection, and may increase within 3-10 days after infection. The papule is painless and does not itch. The inside of the papule may fill with fluid, then a crust may appear, and in the end only a scar will remain, similar to chickenpox. The papule persists for 1-3 weeks, but may go unnoticed or, by mistake, you may attribute it to an injury or bruise.
Over the course of 1-3 weeks, lymph node swelling develops in a single node or group of regional nodes near the site of the bite or scratch. Swollen lymph nodes are often found under the arms, in the neck, or in the groin area. These nodules usually become very tender and the surface of the skin may appear red. Pus may develop in the corresponding lymph nodes. Lymphadenopathy (a condition of enlarged lymph nodes) remains regional and usually resolves within 2-4 months, but can last up to 6-12 months. Rarely, the condition may persist for a year or more.
This is interesting: Bloom's syndrome - photos, symptoms, treatment methods
Other symptoms of cat scratch disease may include:
- pain and general discomfort
- fatigue
- headache
- fever
Less common symptoms include loss of appetite, sore throat and weight loss. In some cases, chills, back pain and abdominal pain may occur.
In children, inflammatory processes appear in the liver (granulomatous hepatitis) or spleen and bone infection. Other atypical manifestations of cat scratch disease include:
- bacillary angiomatosis
- encephalopathy
- inflammation of the retina and optic nerve of the eye
- conjunctivitis
- endocarditis
Eye damage occurs in approximately 5% of patients. Symptoms include a red, irritated eye (similar to conjunctivitis), fever, and enlargement of nearby lymph glands, often in front of the ear.
Neurological complications occur in approximately 2% of infected patients, with encephalopathy being the most common. Symptoms appear after 2 - 3 weeks. In almost all patients, neurological complications resolve without treatment.
Carrion's disease
Carrion's disease, caused by the bacterium Bartonella, is a rare infectious disease. New cases of the disease were found in people who had traveled to other parts of the world; infection is practically not found in Russia or European countries.
In most affected people, Carrion disease is characterized by two clearly defined stages: a sudden, acute phase known as Oroya fever, and a chronic, benign skin abscess. The first stage usually develops approximately 3-12 weeks after the bacteria enters the human body.
Oroya fever can be characterized by high fever, excessive sweating, headache, chills, weakness, and pale skin. In addition, many affected people may develop mental changes, including confusion and disorientation, or even coma. Such disorders occur due to a rapidly developing decrease in the level of red blood cells due to bacterial invasion and destruction of these cells. The first phase of the disease is very similar to malaria .
Additional associated symptoms may include abdominal pain, severe muscle pain, lymphadenopathy, inflammation of the brain and its protective membranes, seizures, and other abnormalities. In addition, some victims may develop chest pain due to insufficient oxygen supply to the heart muscle (angina), thrombocytopenia, difficulty breathing (dyspnea), and impaired digestive and liver function.
Quintan
Bartonella quintana can trigger the development of trench fever, the symptoms of which appear within a few days after the bacteria enters the body. Affected people may develop:
- sudden fever
- chills
- weakness
- headache
- dizziness
- pain in legs and back
This is interesting: Bloom's syndrome - photos, symptoms, treatments
The initial fever can last about four to five days and can recur several times, with each episode lasting about five days. Other symptoms may include a temporary skin rash consisting of flat or raised lesions and an enlarged liver or spleen. Trench fever is usually a self-limiting disease, although relapses and chronic bacterial conditions are known. Severe forms of Volyn fever are seen only in people with weakened immune systems, such as people with HIV/AIDS.
Diagnosis of the disease
After comparing the results of the general examination with a survey of the owner of the sick cat, the doctor prescribes:
- clinical blood test;
- smear to determine hemoparasites.
If infectious anemia is suspected, additional diagnostics are carried out for diseases with similar symptoms:
- viral leukemia (FeLV);
- feline immunodeficiency virus (FIV).
Methods for determining hemobartonellosis:
- Light microscopy of a stained blood smear is the easiest way to identify this disease in cats. Small round parasites are visible on the surface of red blood cells as single inclusions or groups of 2–6 pieces. The edges of the red blood cells become jagged, with raised areas. However, microscopy of a smear often gives a false result if the laboratory worker made a mistake when staining.
- Cytological examination is more reliable, but there is an important feature here too. When preparing the sample, it is correct to use heparin as a stabilizer. If you add EDTA, hemobartonella will break away from the membranes of red blood cells, and their presence will become impossible to determine. Blood counts for hemobartonellosis in cats: hematocrit below 20%;
- red blood cells 2.0–3.5;
- ESR reaction exceeds 38;
- platelets below 200;
- normoblasts are present.
Video: red blood cells infected with hemobartonellosis under a microscope
Development mechanism
After entering the animal’s blood, hemobartonella begins to multiply rapidly, affecting an increasing number of red blood cells and cells of the liver, spleen, and bone marrow. As a result of this process, red blood cells are destroyed. And this, in turn, leads to a drop in the level of hemoglobin in the blood and depletion of the liver. Part of the hemoglobin enters the urine, and it turns red and even brown. Cells and tissues begin to lack oxygen, acid-base balance is disrupted, and acidosis develops. Oxygen starvation causes the appearance of diathesis hemorrhages and degeneration of parenchymal organs.
Did you know? in the USA who gave birth to 420 kittens in her entire life. And in the UK, a kitty named Antigone had the largest litter recorded - 19 cubs.
Problems in metabolism lead to poisoning of the body with toxins that it produces, inflammation and hemorrhages in various organs and tissues. The clinical picture of the manifestation of all the above processes is fever, diarrhea, vomiting, cardiovascular and gastrointestinal syndrome.
The development, spread and manifestation of infectious anemia depends on the state of the immune system of the infected animal.
Treatment of hemobartonellosis in cats
For drug therapy of the disease, the doctor prescribes:
- Tetracycline antibiotics. Doxycycline hydrochloride is administered at a dosage of 10 mg/kg of cat's body weight once daily for at least 2–4 weeks. Be sure to support liver functions with Heptral. The animal is given medications along with food or liquid to reduce irritation of the esophagus. In the first week of treatment, the number of parasites decreases, and hematocrit values increase. When using doxycycline hyclate (for example, Ronaxan) for a pet weighing 4 kg, 2 tablets are prescribed per day, since one contains 20 mg of the active substance. This form of drug release is convenient when calculating the dosage so that it exactly matches the body weight of the animal.
- If the pet cannot tolerate tetracycline medications, the veterinarian will prescribe enrofloxacin. This is an antibacterial substance from the group of fluoroquinolones for subcutaneous injection. The daily dose is 5 mg/kg of pet's weight or 0.6 ml for an animal weighing 3 kg. The duration of treatment for hemobartonellosis in adult cats is at least 10 days. Baytril is convenient to use, in which the concentration of the active substance is 2.5% or 25 mg in 1 ml of solution. You should not use a medicine with a higher content of enrofloxacin, so as not to make a mistake in the dosage. Animals tolerate the drug well, its effectiveness is the same as doxycycline. The dose should not be increased under any circumstances, otherwise the pet will lose its vision. Enrofloxacin is contraindicated in pregnant cats and young animals under one year of age. It is prohibited to use simultaneously with tetracyclines and chloramphenicol.
- To maintain the vitality of the pet and stimulate the regeneration of dead red blood cells, Gamavit and other multivitamin preparations are used intravenously. Compounds containing iron and calcium are prescribed by injection. Antibiotics block the absorption of macroelements from the intestines, so iron salts in pill form are ineffective.
Photo gallery: drugs prescribed for hemobartonellosis
Veterinarians prescribe the unique drug Gamavit to combat infectious diseases and animal intoxication.
Enrofloxacin destroys parasitic bacteria in the blood of pets
Doxycycline hyclate tablets are used to treat hemobartonellosis in cats.
The course of hemobartonellosis is aggravated by concomitant diseases of domestic cats and mixed parasitic infestation. The ability of the bone marrow to regenerate red blood cells is important. If viral immunodeficiency is detected along with hemobartonellosis, the prognosis is generally favorable. If infectious anemia develops against the background of viral leukemia, recovery will not occur. Only short-term improvement is possible, so veterinarians recommend euthanizing the sick animal.
Unfortunately, with a latent form of hemobartonellosis, the pet suffers for a long time from a lack of oxygen. His body adapts to anemia at some point. And the owner notices the disease in the animal only after a sharp weight loss and change in behavior. Doctors are doing everything possible to save him, but treatment does not help if hemobartonellosis is already at the last stage. The drugs used to get rid of the parasite are toxic, and the sick cat is already too weak.
A transfusion of red blood cells will temporarily support vitality, but this type of medical care is only available in large cities. In addition, the response to therapy for hemobartonellosis is too individual. The same drug works in one case, but not in another. The reason for this is still not known. Therefore, in the treatment tactics of hemobartonellosis, there are more questions than answers.
Treatment of adult animals
Treatment of hemobartonellosis in cats includes both the fight against the causative agent of the disease and the removal of symptoms associated with the disease.
Animals are prescribed:
- tetracyclines – Tetracycline, Oxytetracycline, Doxycycline;
- Baytril;
- iron supplements;
- vitamins;
- sedatives;
- droppers, the action of which is aimed at eliminating dehydration;
- Prednisolone to relieve anemia;
- hepatoprotectors to support the liver;
- blood transfusion.
The duration of treatment is 2-4 weeks. After recovery, cats usually become carriers of the disease. Cases of relapse are rare.
Attention! Without adequate treatment, cats with hemobartonellosis die in 30% of cases.
How to treat infectious anemia in kittens
Kittens can become infected with hemobartonellosis when moving to a new owner. Their immune and hematopoietic systems are still weak. Their disease is very severe and usually ends in death. General exhaustion causes cardiac arrest. It is not recommended to treat infectious anemia in kittens with doxycycline, since the drug accumulates in bone tissue, disrupting the formation of the skeleton and teeth. Enrofloxacin cannot be used due to toxicity, which causes vomiting and skin necrosis at the injection site in children. Doctors immediately warn the owner that the prognosis for the outcome of the disease is unfavorable.
All that remains is to try to cure the kitten with the help of antiprotozoal drugs, which are used to prevent parasitic infections. Here, much depends on the type of hemobartonellosis strain. If the disease develops slowly, then there is a chance to save the animal. The main thing is the ability of the drug to disrupt the life of a bacterial cell at a minimum concentration.
A solution of imidocarb dipropionate, which has no embryotoxicity, is suitable for this. It is used once, because the therapeutic effect lasts up to 5 weeks. Dosage - less than 0.1 ml of 4% solution per 1 kg of kitten weight. Inject under the skin with an insulin syringe into the withers area. After 5 days, a blood test is taken. An increase in red blood cells and hemoglobin means victory.
If this does not happen, and the pet’s condition worsens, do not torture the animal and agree to be euthanized. Unfortunately, there is no reliable information about the recovery of kittens from hemobartonellosis after ineffective use of imidocarb.
Is it dangerous for others?
Cat owners are often interested in how dangerous an infectious disease contracted by their pets can be for them. That is, for people. Experts reassure. Their opinion on this issue is unequivocal - no. A cat with hemobartonellosis in its body is not dangerous to its owner. He does not need to check with his doctor after the pet. In addition, since the cat does not pose a danger, there is no need to isolate it from people living in the house. The disease is not classified as a type of zooanthroponosis. It is unique to cats.
To fully ensure your safety when in contact with an infected animal, the owner only needs to remember that hemobartonellosis in cats is an infectious anemia. This means individual choice of disease. If there are other animals in the house: dogs, hamsters, guinea pigs, you don’t have to worry about their health. They won't get infected from a cat. They can catch a disease with a similar name from other sources.
Caring for a sick animal
A pet with infectious anemia does not need to be isolated in a separate room, since the disease is not contagious. The bed is taken to a warm and quiet place to ensure peace for the animal. The litter tray is not moved, but they monitor whether the pet uses it. The animal can urinate on itself due to weakness, so prepare a second sleeping place in advance.
To speed up recovery, you need a diet containing special heme iron (found in animal products). The substance is the basis for the formation of hemoglobin in all mammals. The amount of food is at least 200 grams for an adult animal per day.
Composition of the diet for the treatment of hemobartonellosis:
- beef meat and liver;
- pork lungs and heart;
- cattle blood.
It does not matter whether the food is given raw or cooked. It is important that food is not frozen before cooking. In this case, meat food retains all its beneficial properties. If there is a complete refusal to eat, the owner has to force-feed the cat.
Fighting the animal will only weaken it further, so intravenous nutrition with protein hydrolyzate in a hospital setting is preferable.
A pet exhausted by illness does not lick itself, so the owner takes care of its fur. It is carefully combed out and moisturized if necessary. More difficulties arise if you often have to give your cat tablets (capsules). The animal refuses the powdered medicine mixed with food. Therefore, a device called a tablet dispenser or piller is used. It is used to place a dragee or tablet directly into the cat's mouth along with broth or water to make swallowing easier.
Taking medications with a tablet dispenser facilitates the process of treating a cat for hemobartonellosis
The device acts like a syringe, saving a person’s fingers from scratches and bites of a sick animal. Veterinarians will always help the owner learn how to use the peeler correctly.
Forecast
If left untreated, the cat will be sick for three to eight weeks in the spring, and for one to two months in the fall. In the summer, she may experience weight loss, depression, and shortness of breath.
If the sick animal is isolated in time and treated, the results of therapy are likely to be successful. The outcome of therapy depends on several factors:
- duration of the disease;
- presence of complications;
- infection with FeLV or FIV viruses.
A rare (1%) but possible outcome is death; without treatment, about 25% of affected animals die.
If therapy does not produce the required effect, the disease may return or go into a passive form, into the carrier stage.
If you seek veterinary help in a timely manner, make a competent diagnosis and prescribe medications, the outcome of the disease is positive.
Prevention of infectious anemia
Regular treatment of your domestic cat with drugs against blood-sucking insects will reduce the risk of infection with hemobartonellosis to a minimum. To do this, use drops on the withers, sprays containing repellents and acaricides. A day before going outside, put a collar on your pet to protect against ticks and other parasites.
Unfortunately, strict adherence by owners to the rules for keeping pets does not always protect against parasitic diseases. Well-fed fleas, having jumped off a homeless animal suffering from infectious anemia, live for weeks in the grass or entrance. Ectoparasites easily get on human clothing and infect a pet. The main measure to prevent the spread of hemobartonellosis is disinsection of the habitats of stray cats. These are basements and ground floors of apartment buildings, cellars in country houses. Rodents also live there, whose blood serves as food for fleas. Even without contact with stray animals, a pet runs the risk of developing infectious anemia if fleas are not eliminated in residential buildings.
Infectious anemia in cats is a parasitic disease that is difficult to control. Therefore, pay more attention to its prevention in your pet. A caring attitude towards the health of the animal will allow you to notice external signs of hemobartonellosis earlier. Then the treatment will be successful.
Vaccination and prevention
There is no vaccine against this disease, so the only way to prevent it is regular treatment against blood-sucking parasites. Acaricidal and repellent preparations are produced in the form of drops, sprays and collars. Each of them has its pros and cons, which you should familiarize yourself with before purchasing.
Also try to avoid contact with stray animals. They are often infected with parasites and can infect your pet even after short-term contact. Parasites can be brought into the house on your own shoes or clothes, so the quality of disinfection of basements in apartment buildings plays a big role. On this issue, you can contact the management company or seek private services.
Feline infectious anemia is a dangerous parasitic disease that is often fatal. To protect your pet, it is important not to forget about preventative treatment and seek help with any changes in habitual behavior. The earlier the infection is diagnosed, the greater the chance of a favorable outcome without complications.
The article is for informational purposes only. Contact your veterinarian!
How animals become infected with hemobartonellosis
Pets become infected in different ways. Through bites of relatives - carriers of the pathogen, scratches, injuries. Therefore, males are more often susceptible to the disease: cats are prone to fighting, and females are more careful. But in general, individuals of both sexes are not protected from infection with a blood-parasitic disease. Hemobartonellosis infection is also transmitted by blood-sucking fleas and ticks. The likelihood of the causative agent of hemobartonellosis entering your pet’s circulatory system is high; the disease is widespread.