Clinical signs and diagnosis
Post-vaccination sarcoma is a very characteristic tumor that an experienced veterinarian should suspect without additional research after examination.
- The fact of vaccination or other injections is that a tumor can appear both several months and several years after vaccination.
- It is located in the place where the injection was made (most often - the withers, between the shoulder blades, less often - the thigh).
- Post-vaccination sarcoma does not occur in very young or old individuals; its average age is from 6 to 11 years.
- The tumor is dense, painless on palpation, with clear boundaries.
- Sudden rapid growth.
Often, owners are aware of the presence of a tiny, dense nodule on a cat's withers, but are unaware of the need to see a doctor. Then this formation begins to grow so quickly that the veterinarian already sees a huge mass that rises above the shoulder blades, like a hump. Along with the size of the tumor, the volume of surgical intervention increases and the prognosis worsens. Sarcoma reaches a diameter of several centimeters in just a few weeks.
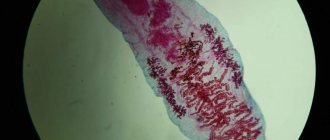
Cytology (the study of tumor cells under a microscope) is used to confirm the diagnosis. The material is taken without anesthesia using a regular syringe. If you need to clarify the size of the tumor and its location, a computed tomography or x-ray is done. The pictures show whether the bones (spine, shoulder blades) are involved in the tumor process.
Before starting treatment, you will need studies of the whole body:
- ECHO of the heart;
- X-rays of light;
- Ultrasound of the abdominal cavity;
- clinical and biochemical blood tests;
- as well as other tests that the attending physician deems necessary.
conclusions
To summarize, we would like to dwell on our own mistakes encountered in the treatment of soft tissue sarcomas in dogs and cats. Firstly, this is an incorrectly calculated volume of the operation. As practice shows, sometimes a surgeon, following the instructions of the owners, may sacrifice the radical nature of the operation in order to reduce the invasiveness of the intervention. Such cowardice can cost the patient’s life, because a recurrent tumor, as a rule, has a higher degree of malignancy and more often metastasizes. Secondly, it is not correct to refuse chemotherapy in the case of high-grade sarcomas (G3) or in the presence of a diagnosis of rhabdomyosarcoma. We know from our own experience how painful it is to discover distant metastases after complex surgery and successful rehabilitation of an animal. Adjuvant chemotherapy should not be delayed, as this allows tumor cells to successfully divide and metastasize. And, in conclusion, I would like to warn against making decisions about euthanizing an animal only on the basis of a cytological diagnosis. In our practice, there were enough cases when, after removing a tumor and conducting a histological examination, the prognosis significantly improved, and the patient lived happily ever after. I hope our experience will help our colleagues and they will successfully treat their patients with this complex and aggressive neoplasm.
Diagnosis of cancer
If there is any suspicion of the presence of a disease, the following studies are carried out:
- Blood and urine tests to evaluate organ function.
- X-ray. Helps detect the presence of metastases in the animal’s body.
- Ultrasound. Using this method, the presence of a tumor can be detected.
- Biopsy. This is done in different ways: tumor cells are taken using a special syringe or endoscope, or during surgery material can be taken for examination. This is the most accurate method for diagnosing the disease.
Clinical manifestations
It is useful for all owners to know how sarcoma manifests itself in cats. This will help detect the disease at an early stage. The main thing, even at the slightest suspicion, is to immediately contact a veterinary clinic for an examination.
So, let's look at the signs of sarcoma:
- Problems with movement, often lameness.
- Decreased activity.
- The appearance of tumors, after a certain time they increase.
- Fracture of limbs.
- Decreased appetite or complete refusal to eat, resulting in anorexia.
- Severe painful spasms, due to which the animal’s behavior radically changes. It is imperative to take painkillers, as the pet may die from pain shock.
Symptoms
An animal suffering from this disease most often experiences the following symptoms.
- The animal limps when walking and may then begin to limp.
- Kisa is rapidly losing weight.
- The appearance of a rapidly growing tumor.
- The animal may completely refuse to eat.
- The cat experiences severe pain, which deprives it of peace and sleep. In some cases, the cat even dies from painful shock.
- Great lethargy, the animal sleeps almost all the time.
Preventive measures
There are no specific preventive measures. The only thing that can be recommended to owners is to limit exposure to carcinogenic substances as much as possible. Also, do not forget about strengthening your immune system. Currently, stores sell a variety of vitamins and complex supplements that will help your pet’s diet become complete. You should not refuse vaccination, because injections can be given intramuscularly.
READ International transportation of animals, general rules for transporting animals to or from Russia
It is important to understand that sarcoma cannot be treated at home. Moreover, there are no effective folk methods to combat it. The owner will only lose precious time, but will not save the life of his pet.
Pathogenesis
Based on morphological and immunohistochemical data, vaccine-induced sarcomas arise from primary mesenchymal cells that have characteristics of fibroblasts and myofibroblasts. The exact origin of myofibroblasts is controversial, but many believe that they represent a "transitional stage" through which fibroblasts or some primary mesenchymal cells pass during the wound healing process. Vaccine injection usually causes a local granulomatous reaction that varies in severity and duration depending on the vaccine and adjuvant.
An increase in the incidence of fibrosarcomas in cats began to be observed in the late 1980s, shortly after the introduction and widespread use of lethal, aluminum-containing rabies and feline leukemia virus vaccines, which had not previously been used in cats. Masu 1996 documented that these vaccines systematically caused palpable inflammatory tumors in cats at the site of injection. Presumably, post-vaccination sarcomas may result from inappropriate or extreme inflammatory or immunological reactions associated with the presence of vaccine components in the vaccination site, which led to uncontrolled growth of fibroblasts and myofibroblasts. Although feline leukemia virus (FLV) and feline sarcoma virus (FSV) cause many diseases and neoplasms in cats, these viruses do not appear to play an important role in the pathogenesis of post-vaccination sarcomas (Elliset et al., 1996).
Research projects conducted in the laboratory of the author and other scientists focus on growth factors and oncogenes as possible participants in this transformation of neoplasms. Many studies and experiments conducted on animals support the hypothesis that growth factors contribute to the transformation of neoplasms. A large percentage of human tumors have been shown to possess receptors for growth factors that they themselves produce in an unusual or autonomous manner. Using immunohistochemical methods, the author and his colleagues documented this phenomenon called autocrine stimulation in post-vaccination sarcomas in cats. In addition, various oncogenic products are homologous to growth factors, their receptors, or other components involved in the growth factor-induced cell transduction signal. It has been proven that increased expression of oncogenes and their healthy copies, protogens, leads to neoplastic transformation of cells. The c-jun proto-oncogene, which encodes a transcriptional protein involved in cell growth and tumorigenesis in vitro, is isolated in increased amounts in post-vaccination sarcomas in cats. Lastly, dysregulation of p53, a tumor suppressor protein, is common in many feline fibrosarcomas, including those associated with vaccination (Helfand et al., 1995). It is clear that differences between the patient's genome and changes in oncogene and growth factor expression play a role in the pathogenesis of these tumors and should be a central focus of future research.
Stages of development
Otodectosis in cats: treatment, drops, drugs
All cancer diseases have several stages of development. They directly affect prognosis and treatment methods.
- First stage. The disease cannot be detected by symptoms due to their absence. Formations are felt that have clear boundaries but are small in size (up to 5 cm). Diagnosis at this stage gives most animals a chance for recovery. The tumor is treatable.
- Second stage. The neoplasms are larger than 5 cm in size. The clarity of the boundaries is lost. There is a rapid increase. Metastases are not formed.
- Third stage. The lymph nodes that are located next to the tumor are affected. This tumor is much less treatable.
- Fourth stage. The last and most dangerous. Metastases spread to all organs of the cat. Therapy is selected to alleviate the pet’s condition.
Important! At stage 4, surgical removal of sarcoma in a cat is justified, provided that it significantly improves the patient’s quality of life, for example, it removes pain.
Is sarcoma dangerous for humans?
The nature of cancer is not yet fully understood. Theoretically, sarcoma can be contagious and transmitted to animals or people. However, there is an opinion that if oncology were contagious, all oncologists would die out. Therefore, there is no need to worry.
Surgery can prolong a pet's life for many years to come. The disease is really dangerous for his health, but it is worth fighting for his future and treating him even if it seems that there is no hope.
Treatment algorithm for soft tissue formation
If the tumor extends beyond the musculofascial boundaries, the surgeon should be guided by the principles of zonation and blocking. This is especially true when removing sarcomas that have a lymphatic metastasis route, primarily rhabdomyosarcoma, histiocytic sarcoma and hemangiosarcoma. Such tumors should be removed en bloc, including all tissues in the area of regional lymphatic drainage. The presence of tumor cells in regional lymph nodes is a poor prognostic factor. However, enlargement of regional lymph nodes does not indicate the presence of tumor cells in them. We encountered a case where, after a histological examination of removed enlarged lymph nodes in dogs with soft tissue sarcoma, no tumor cells were found and a diagnosis of reactive hyperplasia was made. We did not prescribe systemic chemotherapy to such patients.
When surgically removing soft tissue sarcomas, antiblastic techniques can be used. In our practice, we tried intraoperative irradiation of the surgical wound and the intraoperative use of photodynamic therapy. The use of ionizing radiation intraoperatively is associated with great technical difficulties, since the source of ionizing radiation is located outside our clinic. We also encountered a lengthening of the postoperative period and complications during the healing of the surgical suture.
When using photodynamic therapy intraoperatively, we administered to the patient a dose of photoditazine 1 mg/kg body weight 1 hour before surgery. The tumor was removed and the tumor bed was irradiated with a laser with a wavelength of 661 nm. Of the postoperative complications, only swelling of the surgical suture on days 3-7 and the presence of seroma were noticed.
Among the technical difficulties, it should be noted that the patient needs to stay in a dark room for 24 hours after photodynamic therapy. After surgery, the removed material should be sent for histological examination.
The main prognostic factor is the presence of tumor cells at the resection margin. In order for a morphologist to be able to reliably determine their presence, it is necessary to paint all surfaces of the specimen that came into contact with body tissues before fixation with a special paint. When it is impossible to present all the removed material for examination, the most suspicious areas should be marked with paint. If tumor cells are found in the stained areas, the operation is considered non-radical and the animal requires additional treatment. The most effective is a repeat operation, with excision of the surgical scar and capture of 5 cm of tissue in each direction; postoperative irradiation of the resection margins and surrounding tissues can also be used. We use adjuvant radiation therapy for positive resection margins, for rhabdomyosarcoma, and for high-grade sarcomas - G3. We begin radiation therapy no later than 10-14 days after surgery at a dose of SOD 50-60 Gy. The dose per fraction is 5 Gy. Wide irradiation fields are used, departing 5-7 cm from the resection boundaries. Radiation therapy sessions are carried out 3-5 times a week, using sedation. The session time is usually 5-10 minutes; short-acting drugs are used for sedation: pofol and domitor with antisedan. We had no complications associated with anesthesia.
In humane medicine, preoperative irradiation is widely used in the treatment of soft tissue sarcomas. Its tasks are:
• reduction of the malignant potential of the tumor due to the death of the most aggressive cells;
• total damage to subclinical tumor foci;
• reduction in tumor volume.
The interval between the course of radiation therapy and surgery should be no more than 2-3 weeks. Because of this, after neoadjuvant radiation therapy, a large number of postoperative complications are recorded, up to 40%. When comparing preoperative and postoperative radiotherapy for soft tissue sarcomas, no statistically significant difference in effectiveness was found. In our practice, we use only adjuvant radiation therapy.
In the treatment of high-grade (G3) soft tissue sarcomas, especially in the case of histologically confirmed histiocytic sarcoma, lymphangiosarcoma, synovial sarcoma, hemangiosarcoma and rhabdomyosarcoma, we use adjuvant chemotherapy. Doxorubicin alone or in combination with cyclophosphamide is used as a chemotherapeutic agent. According to a meta-analysis of randomized trials in humane medicine, doxorubicin reduces the risk of local and systemic recurrence with a trend towards increased survival, which was better observed when the tumor was localized to the extremity. However, such studies have not been conducted in veterinary medicine. Other combinations of doxorubicin have not shown greater effectiveness compared to doxorubicin alone.