Addison's disease (hypoadrenocorticism) is an endocrine pathology accompanied by a low level of synthesis of corticotropic hormones. It is typical for middle-aged animals, more often diagnosed in females, among breeds - poodles, Rottweilers, terriers, Great Danes, and collies. With Addison's disease in dogs, there is a serious disruption in metabolism - an imbalance of the buffer system, there is a loss of potassium and accumulation of sodium in the cells.
Causes of the disease: genetic failure in the endocrine system, injury to the pituitary gland, inflammatory processes in the brain, tumors, neoplastic neoplasms of the kidneys and adrenal glands (lymphoma). It is also diagnosed due to long-term treatment with glucocorticoids without monitoring the biochemical parameters of the dog’s body.
It is difficult to identify in a timely manner , since the signs are nonspecific. Main symptoms: lethargy, weakness, reluctance to do exercises, refusal of long walks, active games; in advanced cases, severe depressive state, up to the development of lethargy; loss of appetite, weight, with prolonged progression severe exhaustion, but increased thirst; the coat is dry, disheveled; dry skin, sometimes dandruff; increased urination; sometimes vomiting, diarrhea, constipation, blood in feces; pain in the peritoneum; heavy breathing, shortness of breath; hypothermia, seizures and even coma.
Constipation
Diagnosis of the animal: general and biochemical blood test, ultrasound of the heart muscle and kidneys (with adrenal glands), X-ray examination, ECG. The diagnosis is considered established when the concentration of cortisol in the blood is more than 2 mcg/dl. If it is below this indicator, then the veterinarian conducts a test with adernocorticotropic hormone. The study can confirm the diagnosis of Addison's disease and also exclude Cushing's syndrome.
Treatment of Addison's disease is determined by the phase of the disease. If in the acute stage, the dog experiences a state of shock and convulsions, then intravenous injections of cortisone (dexamethasone) are administered. In order to improve the dog's condition, it is wrapped up and warmed with a heating pad and bottles of warm water. If high levels of potassium in the blood are accompanied by bradycardia, injections of insulin and dextrose are prescribed.
In the chronic stage, in most cases, treatment is reduced to symptomatic therapy. An important place is occupied by the correction of electrolytic balance in the body. For this purpose, Percorten and Cortineff are prescribed. Before taking the drug, a biochemical blood test is performed to determine the level of potassium and sodium. Lifelong administration of Cortineff requires monitoring blood counts at least once every six months.
Prednisone helps maintain the required level of cortisol in the blood of dogs. An analogue of the adrenal hormone is prescribed in minimal doses with mandatory monitoring of blood biochemistry once every 6 months and dosage adjustment.
Treatment is prescribed for life.
Read more in our article on Addison's disease in dogs.
What is hypoadrenocorticism in dogs
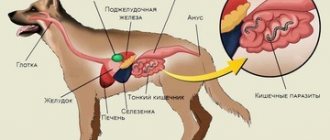
Hypoadrenocorticism develops when the adrenal glands, the endocrine glands located directly above the kidneys, malfunction. They are responsible for maintaining metabolic processes with the help of 2 important hormones:
- cortisol, or hydrocortisone, responsible for suppressing stress and regulating carbohydrate metabolism;
- aldosterone, which ensures the regulation of water and electrolyte balance.
If a hormonal deficiency occurs, a four-legged patient is diagnosed with Addison's syndrome, and if a surplus occurs, Cushing's disease. Both conditions are equally dangerous for the body.
Without timely assistance, a sick dog may die from hypovolemic shock. This condition is characterized by a rapid reduction in blood volume due to dehydration caused by uncontrolled vomiting and diarrhea.
What kind of syndrome is this?
Addison's disease or hypocortisolism is a complex endocrine disease. Its essence is the pathologically insufficient production of glucocorticoid and mineralocorticoid hormones by the adrenal cortex.
In Addison's disease, the adrenal glands produce catastrophically little steroid hormones, in particular cortisol. And this hormone affects the entire metabolism of proteins, fats and carbohydrates. Accordingly, for the optimal balance of glucose in the blood. With hypocortisolism, potassium is rapidly removed from the dog's body, sodium is retained - all biochemical parameters of the blood are severely disturbed.
In world veterinary medicine, this disease has been called the “great simulator” for several decades. This rather strange name for medicine is due to a single factor: when diagnosing hypocortisolism, the pathology can be mistaken for any other problem.
Causes of the disease and predisposition of the animal
Addison's disease is classified as a congenital pathology, but in addition to genetic predisposition, there is also a breed predisposition. Most often the disease affects:
- Rottweilers;
- Border Collie;
- West Highland White Terriers;
- Great Danes;
- royal poodles;
- basset hounds.
Sometimes this syndrome develops in other breeds, so do not let your guard down. The following factors become the trigger for the development of this disorder:
- long-term or improper treatment of Cushing's disease, which suppresses the production of both hormones;
- bleeding disorders and adrenal infarction, reducing blood supply to the endocrine glands;
- autoimmune disorders accompanied by the destruction of one’s own cells;
- fungal, viral and bacterial infections affecting the endocrine system;
- surgery to remove the adrenal glands;
- diseases of the pituitary gland and hypothalamus, complicated by adrenal dysfunction.
In addition to genetic and breed predisposition, it is important to note gender and age. The risk group includes all females aged 1.5 to 2 years. Unlike a number of other pathologies, sterilization during hypoadrenocorticism is not an effective prevention. Sterilized pets and those actively involved in breeding are equally vulnerable.
What is this disease?
This is a deviation in the functioning of the endocrine system, which occurs due to a disruption in the process of hormone synthesis. This is one of the causes of the disease, but it is not the only one. Another reason for the development of pathology may be long-term use of glucocorticoid drugs. The symptoms of this disease are very vague and therefore difficult to determine. This often leads to a false diagnosis. The disease is congenital, so young dogs suffer from it, or rather it manifests itself in young dogs under 1 year of age. Probably, if the veterinarian begins to remember some of the symptoms of adrenal diseases, he will understand that the diagnoses could not have been made correctly, and in some cases Addison's disease could have been diagnosed. This disease is quite secretive and similar to many others. Therefore, its diagnosis is quite complex and requires a large number of accurate tests. What, then, are the classic signs of hypoadrenocorticism? If we start to understand the typical form of the disease, then, most likely, we will encounter a young dog that may periodically experience gastrointestinal distress for a long time. At the same time, the dog will be lethargic and lag behind in body growth and development. At the first stage of the disease, you can see a deterioration in the dog’s health. At an advanced stage of Addison's disease, dangerous symptoms appear. In both the first and second cases, it is necessary to quickly take the dog to a veterinary clinic and have it examined by a knowledgeable doctor. This disease does not tolerate slowness and procrastination.
[custom_ads_shortcode3]
Forms of the disease
Depending on the cause and symptoms present, hypoadrenocorticism is divided into several types. The most insidious is atypical.
Primary
This form occurs when the glands are directly affected and reduces the production of both hormones at the same time. The patient has hyperkalemia and hyponatremia - pathological conditions characterized by excess potassium and lack of sodium.
Secondary
Develops as a result of congenital or acquired diseases of the pituitary gland and hypothalamus. It is less common than the primary form and affects only the production of cortisol. Water-electrolyte balance is maintained.
Atypical
Accompanied by the appearance of nonspecific symptoms not characteristic of the pathology, or a latent (asymptomatic) course. This makes diagnosis difficult and significantly complicates treatment. For this reason, at the slightest suspicion of an atypical form, the animal must be regularly examined by a veterinarian every six months.
Addison's disease
Author:
Smirnova O. O., Ph.D., veterinary therapist, endocrinologist, Veterinary Clinic of Neurology, Traumatology and Intensive Care, St. Petersburg.
If we ask ourselves how often we encounter Addison's disease in our daily practice, most likely our first answer will be: not often. Is it really? Perhaps we are somewhat mistaken in our understanding, since Addison's disease is one of the most common pathologies of the endocrine system among young dogs. It is possible that in some cases we simply cannot interpret the patient's data to make a correct diagnosis. It is not for nothing that Addison’s disease (hypoadrenocorticism) is called the “great simulator” all over the world - a term that speaks for itself: GREAT - this word does not require synonyms; SIMULATOR – imitator, master of disguise.
According to this scheme, the classic course of a typical form of hypoadrenocorticism develops. But there is a possibility of encountering an atypical manifestation of the disease, associated only with insufficient synthesis of glucocorticoids. In this case, the patient will not develop Addison's crisis in its true sense and will not experience dehydration. The clinical picture will be characterized mainly by periodic gastrointestinal disorders, hypoglycemia, lethargy, and retarded growth and development. Table 2 presents summary data on the characteristics of the main symptoms and physical examination data, depending on what form the patient has.
In addition to the history and characteristic findings of the physical examination, routine laboratory tests will also help us make a diagnosis. It is still important to determine what form of the disease (typical, atypical) we are faced with and whether the patient is in a state of crisis. In the event of a crisis, all routine studies will indicate a state of hypovolemia. In this regard, signs of hemoconcentration with an increase in hematocrit, red blood cell count and hemoglobin are often observed. However, with a long course, the disease is often accompanied by anemia. Express diagnostics
necessary for resuscitation of a patient, includes the determination of the following basic parameters: –
Hematocrit
;
– blood pH
;
– Markers of uremia: creatinine, urea
;
– Concentration of total protein and albumin
;
– Electrolyte concentration: Na++, K+, Cl-
.
Na:K ratio BUT! This change is not a pathognomonic symptom. Approximately 10-30% of dogs have normal electrolyte concentrations at the time of diagnosis. This occurs due to early diagnosis or manifestations of atypical cases of the disease. Important: the diagnosis is not excluded when, in the presence of clinical signs, minor (or no) electrolyte changes are observed. Especially if the patient undergoes diagnostics after infusion therapy. The potassium content in the blood serum at which ECG changes occur varies in different patients, while the sequence of electrocardiographic changes remains the same (it is indicated in the order of occurrence): T wave; QRS complex; change/disappearance of the P wave; waves that resemble a sine curve.
Hyperkalemia can range in severity from mild to severe. A mild degree corresponds to a K+ concentration of 5.5-6.5 mmol/l. In this case, when conducting electrocardiography, usually only an increase in the height of the T wave is characteristic. At a K+ concentration exceeding 6.5 mmol/l, an expansion of the QRS complex and a decrease in QRS amplitude, an increase in the length of P-waves and the PR interval are usually observed. A severe degree develops when K+ is more than 8.5 mmol/l: P-waves can completely disappear, cardiac fibrillation and asystole occur. This degree of hyperkalemia is the most life-threatening and requires emergency care. Visual diagnostic methods play a supporting role in confirming the diagnosis and help in differential diagnosis. When performing an X-ray of the chest cavity, the consequences of hypovolemia are noted: microcardia, microhepatia, narrowing of the lumen of the pulmonary artery of the cranial lobe of the lung, caudal vena cava. Megaesophagus is sometimes combined with hypoadrenocorticism. As this complication develops, characteristic radiographic abnormalities will be noticeable. When performing an abdominal ultrasound, a distinctive feature is often hypoplasia of both adrenal glands. In dogs, the adrenal glands are considered hypoplastic when the left adrenal gland remains the gold standard for confirming the diagnosis. There are several conditions that must be met when conducting the test. The dog should not have received exogenous glucocorticoids before the test (or at least several weeks should have passed since their last use). Only dexamethasone does not cross-react with endogenous cortisol. But dexamethasone inhibits the synthesis of endogenous cortisol after 4-6 hours from the moment of its administration. Accordingly, in case of extreme need for the use of glucocorticoids, dexamethasone can be injected, but the test must be completed no later than 4 hours from the moment of drug administration.
Clinical picture - symptoms
Symptoms of Addison's disease in dogs do not appear until 3-6 months. Until this time, puppies with congenital pathology are no different from their counterparts.
Alarming changes appear only after the overwhelming area of the adrenal cortex is affected. At this point, healthy tissue makes up no more than 15%, and reserve hormones have to be used to maintain metabolic processes.
The speed of development of pathology is individual. Symptoms can gradually increase over several weeks or months, accompanied by a series of remissions and relapses, or appear in all their glory in just a couple of days. The symptoms themselves will depend on the stage of the disease. At the initial stage, the condition becomes more complicated:
- loss of appetite, quickly leading to a distinct protrusion of the ribs and spine due to weight loss;
- increased thirst and frequent urination;
- chronic vomiting and diarrhea with dark feces;
- dehydration (dry coat, dry mucous membranes, lethargy and slow smoothing of the skin after it is compressed);
- apathy and drowsiness.
As the state of health worsens, the symptoms are supplemented by hair loss, attacks of shortness of breath, a decrease in body temperature, abdominal pain on palpation, blanching of the mucous membranes, muscle tremors, a slow pulse and the appearance of blood in the stool. If at least 2 of the listed signs are detected, it is recommended to take your pet to a veterinary clinic as soon as possible.
It will not be possible to make a diagnosis without examination, since all the symptoms that appear are nonspecific and can accompany any other pathologies not related to the endocrine system. The only characteristic sign is hypovolemic shock. It is easily identified by sudden loss of consciousness or stupor. Without emergency resuscitation, death can occur within minutes.
Symptoms of the disease
Clinical manifestations directly depend on the complexity of the course and duration of the disease. If at the first stage of the disease a sick pet shows a slight deterioration in its health, then with an advanced and acute course life-threatening symptoms may appear for the dog.
Among the typical signs characteristic of the initial stage of the disease:
- poor appetite
- diarrhea,
- vomit,
- increased thirst,
- frequent urination,
- sudden weight loss,
- depressive state.
As the pathological condition develops, the animal may experience:
- hair loss,
- low body temperature,
- pale gums,
- weak pulse
- attacks of shortness of breath,
- pain in the abdominal area,
- blood in stool
- lethargy.
If any of the above symptoms appear, you should immediately seek veterinary help. A professional veterinarian will prescribe diagnostic measures to make an accurate diagnosis and course of treatment.
How is the diagnosis carried out?
Veterinarians call hypoadrenocorticism “the great simulator.” Due to the lack of specific symptoms, it is often mistaken for a viral infection or gastrointestinal disease.
In some cases, even laboratory tests do not help. This situation is typical for the primary form with simultaneous damage to the pituitary gland. Due to the maintenance of normal aldosterone levels, test results are often false negative. For this reason, the cortisol level, which undergoes changes in both types, is taken into account when making a diagnosis.
Blood tests
To assess glucose levels, the condition of the pancreas, liver and kidneys, general and biochemical blood tests are taken from the four-legged patient. If there is a disorder, there is a deficiency of sugar and sodium with a surplus of potassium and phosphorus. Also, chlorine, released together with sodium, deviates less from the norm. A secondary infection is confirmed or refuted using an antibody test.
Observation of symptoms
After taking a history, the four-legged patient is examined for the main symptoms. With cortisol deficiency note:
- dehydration;
- tremor;
- hypoglycemia;
- episodic muscle spasms;
- anorexia;
- apathy and weakness;
- stomach ache;
- semi-liquid stool with an unpleasant odor and inclusions of blood.
In case of water-electrolyte imbalance, the symptoms are complemented by bradycardia, reduced capillary refill rate, low pulse, hypothermia and hypovolemic shock. To identify all these symptoms, blood and urine tests, ECG, MRI, ultrasound and x-ray are used.
ACTH test
The most informative and reliable test is the adrenocorticotropic hormone stimulation test, or ACTH. When conducting it, two indicators are compared: the level of cortisol in the normal state and after the administration of ACTH.
If there is a disorder, the hormone level remains below normal in both cases or increases rapidly 30-60 minutes after the injection. If the dog is healthy, then the cortisol value corresponds to the norm immediately after blood collection and increases slightly after administration of the drug, maintaining its position within the reference range.
To obtain more reliable results, it is recommended to carry out the test in the morning, when the hormone level reaches its maximum value. Exceptions include cases where the four-legged patient is in critical condition and requires urgent resuscitation.
How to diagnose Addison's disease?
Although signs of adrenal disease may be difficult to notice as the disease progresses, serious consequences such as shock and signs of kidney failure may appear suddenly.
Veterinarians make a preliminary diagnosis based on the cat's history, characteristic signs, and some laboratory abnormalities, such as very low sodium levels and very high potassium levels in the cat's blood.
Specific adrenal function tests are needed to confirm the diagnosis of Addison's disease.
Adrenal crisis requires emergency medical attention and treatment with intravenous fluids to restore water levels and normal salt and sugar balance in the cat's body. When the cat's condition has stabilized, hormone replacement therapy is often used. In this case, the cat should be under regular observation so that the results of treatment can be assessed and, if necessary, the dosage of medications can be adjusted. For long-term treatment, medications may be given to the cat orally or by injection.
What treatment will the veterinarian prescribe?
Treatment of Addison's disease in dogs is based on eliminating the effects of dehydration, normalizing water and electrolyte balance, stabilizing hormonal levels and stopping bleeding in the gastrointestinal tract. If a four-legged patient is in a serious condition at the clinic, then infusion therapy and emergency blood transfusion are used to provide first aid. For some time he is left in the hospital under intravenous drips with a catheter.
After stabilization of the condition with the help of rehydration and colloid solutions, the patient is transferred to lifelong hormonal therapy. This is necessary to maintain quality of life, since after pathology the organs will never be able to produce the required amount of cortisol and aldosterone.
All medications can be purchased at a regular pharmacy. Only the recommended dosages will differ. A dog's metabolic rate is higher than a human's. To obtain the same effect, animals require a larger volume of the drug, since otherwise the active substances will be eliminated from the body too quickly.
Please note that initial dosages may be adjusted depending on test results. For this reason, you should not be guided by the instructions inside the package or your own conclusions. If you want to keep your pet healthy, do not deviate from medical recommendations.
Hormonal medications must be administered intravenously or subcutaneously, so it is recommended to master the technique of administering these injections or entrust these procedures to the staff of the veterinary clinic. The tablets begin to act on the body with a slight delay, so it is better to avoid their use until the four-legged person’s well-being improves.
You will also have to measure your glucose levels daily. An electronic glucometer will help you cope with this task. The test is quite easy to perform at home by making a small puncture in your pet's ear.
Treatment for hypoadrenocorticism does not involve dietary changes. Particular attention will have to be paid only to stressful situations: changing place of residence, traveling on public transport or operations. To extinguish negative emotions, the dog will need more cortisol, so the dosage of hormonal medications will have to be temporarily increased.
A few weeks before the exciting event, you should be examined by a veterinarian and consult about revising the volume of substances administered. Making a decision on your own is strictly prohibited, since an accidental overdose can result in Cushing's disease.
Treatment
Addison's disease occurs in two forms. The first form is atypical. There is an acute deficiency of glucocorticoids in the body.
The second form is typical. In this case, the dog suffers from a minimum of both glucocorticoids and mineralocorticoids at the same time. Such differential diagnosis is extremely important for further prescription of adequate therapy.
To make a correct diagnosis, it is necessary to collect the most complete history from the owner, take and carefully analyze a biochemical blood test from the dog. Equally important are: ECG, ultrasound of the abdominal cavity (in some cases) and a stimulation test with ACTH (artificial administration of adrenocorticotropic hormone).
If a dog with hypocortisolism is brought to the clinic already in a state of crisis, urgent resuscitation procedures are necessary to:
- infusion therapy (first of all, to restore dehydration of the body);
- correction of electrolyte disturbances;
- elimination of hyperkalemia (introduce insulin and glucose in one mixture);
- correction of hyponatremia;
- blood transfusion (for hemorrhagic anemia);
- eliminating hypoglycemia;
- use of colloidal solutions;
- elimination of severe metabolic acidosis.
Fludrocorizone, Prednisolone and Dexamethasone are among the most popular drugs used as replacement therapy throughout a dog’s life.
Important. The main difficulty in diagnosis will arise if it turns out that hormone deficiency is caused not only by a primary lesion of the adrenal cortex, but also by a secondary lesion of the pituitary gland. In this case, the test results will be falsely normal.
Is it possible to prevent the development of the syndrome?
Due to genetic predisposition, there is no effective prevention. The only way to truly prevent hereditary transmission is to exclude all affected animals and their offspring from breeding. But this is not always feasible, since the first signs of Addison’s syndrome may appear only after 2 years, when sick puppies have long since found new owners.
Conclusion
Hypoadrenocorticism in dogs is a rare but very dangerous disease. When the first symptoms of malaise are detected, the animal should be immediately taken to a doctor, without waiting for specific signs of hypovolemic shock.
The article is for informational purposes only. Contact your veterinarian!